- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
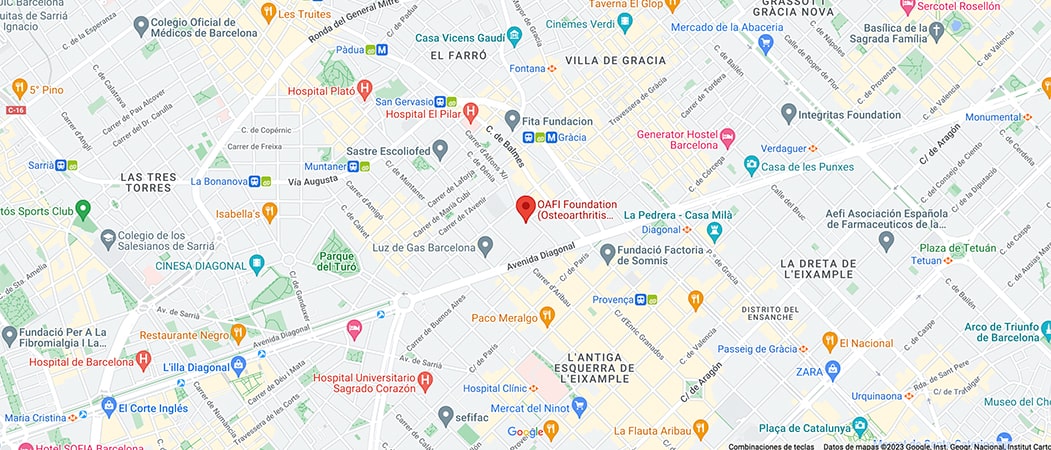
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

-

Weight loss can slow down knee joint degeneration

A study at the University of California claims that obese or overweight people who lost 5-10% of their body weight over a 48-month period significantly decreased knee cartilage degradation. The results of the research have been published in the journal Radiology.
The study involved 640 people with a body mass index (BMI) over 25, who had risk factors for osteoarthritis or were diagnosed with mild osteoarthritis by MRI. The patients were divided into three groups: those who lost more than 10% of their body weight, those who lost between 5 and 10%, and a control group whose weight remain unchanged.
Slows down cartilage degradation
The results show that people who lost 5-10% of their weight had a lower rate of cartilage degeneration compared to the control group. In the group that lost more than 10%, cartilage degradation was much slower.
Researcher Alexandra Gersing from the Department of Radiology and Biomedical Imaging at the University of California, San Francisco (USA) stresses that the results of her study emphasize the importance of including personalized therapy and lifestyle intervention strategies for patients to prevent structural degeneration of the knee joint as early as possible in obese or overweight people at risk for osteoarthritis or already showing symptoms of the disease.
Obesity and Osteoarthritis
According to the US National Institute of Health (NIH), obesity is a risk factor for osteoarthritis. Being overweight or obese puts extra stress on joints and cartilage, leading to increased wear and tear. In addition, people with more body fat may have elevated blood levels of molecules that cause inflammation in the joints, increasing the risk of osteoarthritis.
Article reference
Categories :


















Leave a Reply