- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
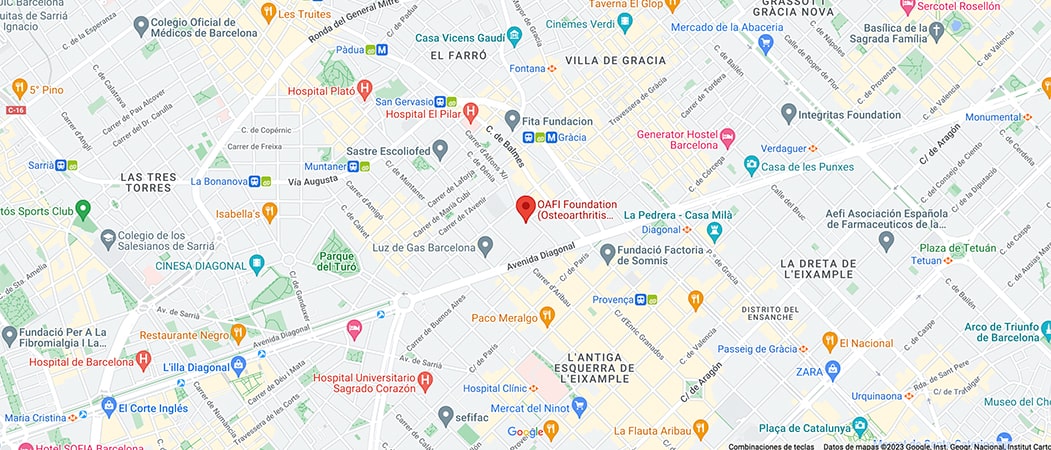
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

-

Prevention and early diagnosis of Osteoarthritis

Article courtesy of Dr. Francisco Castro-Domínguez, Head of Section, Rheumatology Department, Centro Médico Teknon, Barcelona. Coordinator, SER Working Group on Arthrosis, ARTROSER, Spanish Society of Rheumatology.
Introduction
In Spain, osteoarthritis affects around 7 million people and according to the EPISER 2016 study, the prevalence of osteoarthritis in one or more locations in the population over 40 years of age is 29.35%, with the prevalence of lumbar osteoarthritis being 15.52%, knee osteoarthritis 13.83%, cervical osteoarthritis 10.10%, hand osteoarthritis 7.73% and hip osteoarthritis 5.13%.
Historically, osteoarthritis was considered to be a simple degenerative process or wear and tear of the joint, a concept that is still current in popular wisdom.
In recent years, new advances in the understanding of the disease have shown that the origin of osteoarthritis is much more and that what is now understood by the term osteoarthritis (in the Anglo-Saxon world, osteoarthritis is called osteoarthritis) is not the same as osteoarthritis: osteoarthritis is called osteoarthritis itself), is in fact a disease with many different subtypes, which starts with a long preclinical stage (up to 20 years, without symptoms) and of which its final common clinical manifestation is joint pain and dysfunction, which are the symptoms that are unfortunately on the lips of all sufferers of this disease.
The pathways to this joint stage will be different in each subtype of patient, and the pathogenic components, including inflammation, will be present to different degrees depending on the subtype, determined by risk factors, and time of disease progression.
Prevention
Multiple risk factors for osteoarthritis have been identified, including micro-impact (repetitive load handling) or high impact (trauma) joint injury, obesity, sarcopenia (loss of muscle mass), genetics, biomechanical alterations (joint shape and alignment), gender (affects women more) and ageing (affects older people more). Some are modifiable, such as obesity, sarcopenia and inadequately managed workloads, and others are not, such as ageing, gender and genetics.
Prevention of osteoarthritis consists of applying non-pharmacological treatment strategies aimed at correcting modifiable risk factors.
In general, it is recommended to avoid inappropriate handling of loads, weight loss in those who are overweight or obese, daily aerobic physical exercise, exercise to gain muscle mass, and a healthy diet and lifestyle, both of which can act by conditioning epigenetics.
Early diagnosis
In osteoarthritis, all the tissues that form it are altered: cartilage, subchondral bone, synovial membrane, joint capsule, menisci, bursae, ligaments and muscles. The origin and the order in which these alterations occur is different in each patient.
The main symptoms are pain and limitation of joint function. Stiffness, crepitus, swelling, restriction of joint range of motion, joint instability or muscle atrophy may be added depending on the case.
Early diagnosis is very important as it offers the possibility of implementing non-pharmacological strategies aimed at eliminating modifiable risk factors, with the aim of slowing progression, preventing joint dysfunction and enabling pain to be treated more easily and successfully.
In the event of suffering any of these symptoms, you should see your rheumatologist for a clinical assessment and, if necessary, to undergo the complementary examinations that your rheumatologist considers appropriate in your specific case.
Article courtesy of Dr. Francisco Castro-Domínguez, Head of Section, Rheumatology Department, Centro Médico Teknon, Barcelona. Coordinator, SER Working Group on Arthrosis, ARTROSER, Spanish Society of Rheumatology.
Image by Dr. Manuel González Reyes en Pixabay