- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
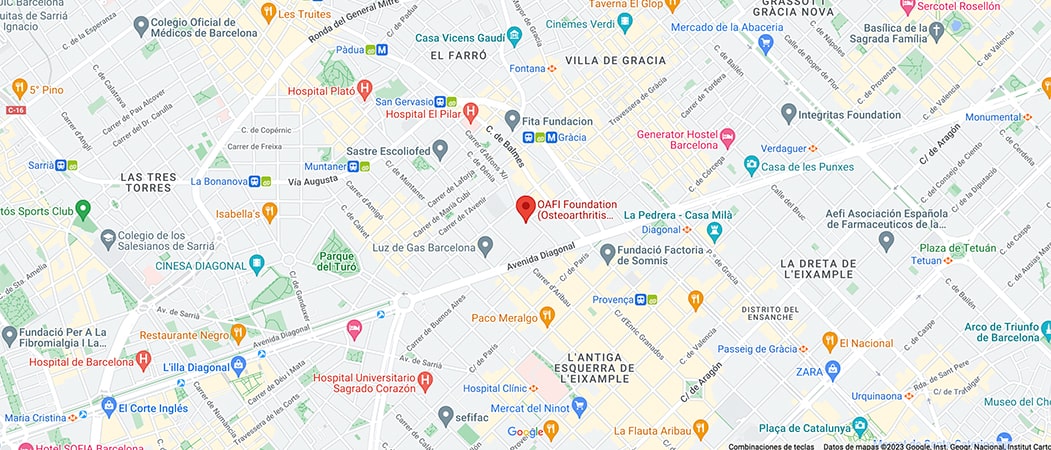
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

-

Arterial hypertension and rheumatic diseases: relationship or interaction?

- Hypertension is the main modifiable risk factor – unlike, for example, age or gender – for vascular diseases such as coronary heart disease (angina pectoris, myocardial infarction), heart failure and stroke, among others.
Article courtesy of Dr. Mariano de la Figuera, Internal Medicine Specialist. Castelldefels Medical Center
Hypertension (HT), defined by a sustained elevation of blood pressure both in the health professional’s office (BP>140/90 mmHg) and outpatient (BP>135/85 mmHg), is the main modifiable risk factor – unlike, for example, age or gender – for vascular diseases such as coronary heart disease (angina pectoris, myocardial infarction), heart failure and stroke, among others. It is estimated that, worldwide, more than 1.25 billion people are hypertensive. The prevalence rate in Spain in people between 30-79% is slightly over 30%, figures that increase with age to over 60% in those over 65 years of age.
With regard to the possible causes of HT, 90-95% of cases are primary forms (essential or idiopathic HT), although the pathophysiological mechanisms responsible for the chronic elevation of BP are increasingly better understood. In clinical practice, around 5% of cases are secondary HT and, therefore, potentially curable. One of the pharmacological causes of BP elevation is the chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) frequently used in joint pathology such as osteoarthritis.
Treatment of Arterial Hypertension
The treatment of hypertension is based on the adoption of certain lifestyles, such as a low-salt diet, weight loss and physical exercise, among others. Pharmacological treatment is the cornerstone of the medicine we practice. The different and very varied drugs for HT are grouped into 5 large “families”: Diuretics (DIU. Example: Hydrochlorothiazide), Angiotensin Converting Enzyme Antagonists (ACEI. Example: Lisinopril), Angiotensin ATII Receptor Antagonists1 (ARAII. Example: Valsartan), Calcium antagonists (Example: Amlodipine) and Beta-blockers (BB. Example: Bisoprolol).
All these drugs, and especially the rational combination among them, have been shown to: 1) significantly reduce BP figures, 2) achieve the goals of HT control in a large number of patients (BP <140/80 mmHg or < in diabetics 130/80 according to the different Clinical Practice Guidelines and 3) the most important and best news: significantly reduce, both in relative and absolute terms, vascular complications and mortality related to HT. In other words, it saves lives. Rheumatologic diseases and ETSRheumatologic diseases and ETS
Rheumatologic diseases and Arterial Hypertension
Focused on the relationship of rheumatologic diseases with the Arterial Hypertension -in both cases these are chronic pathologies– several aspects should be highlighted.
First, in autoimmune rheumatologic diseases (examples: Rheumatoid Arthritis, Psoriatic Arthritis, Systemic Lupus Erythematosus, other autoimmune connectivopathies, Polymyalgia Rheumatica, etc) in which inflammation is the main mechanism involved in their development and evolution, the prevalence of AHT is higher than in the general population. In this sense, it has been speculated that the so-called “vascular/endothelial inflammation” may play a role in the development of vascular complications of HT and some antihypertensive drugs have been shown to improve endothelial function. Therefore, it cannot be ruled out that HT shares some mechanisms with the aforementioned rheumatic diseases.
In any case, there is no evidence that the treatment of autoimmune rheumatic diseases (NSAIDs, steroids, immunosuppressants, biologics, etc.) reduces the incidence and prevalence of hypertension. With regard to degenerative osteoarticular diseases, such as osteoarthritis, any pathophysiological link with HT is speculative. However, two very specific situations, such as overweight/obesity and sedentary lifestyle, are closely related both to primary HT and to some degenerative rheumatic diseases (examples: osteoarthritis of the knee and hip), which has practical implications.
Secondly, and from the clinical-therapeutic point of view it is a relevant issue, there are a number of considerations about rheumatic diseases and HT, so that these should be considered as a special subgroup in the diagnosis, evaluation and treatment of HT.

I will analyze them separately:
Diagnosis of HT
The use of NSAIDs or steroids cannot be considered a cause of HT (sustained elevation of BP), but it does cause transient elevations that make it difficult to diagnose. Therefore, although it is not always possible, these drugs should be withdrawn during the diagnostic phase of HT in order to measure BP under the best conditions. If this withdrawal is not possible and the patient maintains high BP levels, he or she should be considered hypertensive and follow the evaluation and treatment process.
Non-pharmacological treatment
In relation to lifestyle changes, regular aerobic physical exercise (brisk walking, swimming, cycling, dancing, etc) is a very effective measure to reduce BP. However, in joint pathology, especially in advanced forms of knee and hip osteoarthritis, this can be a major limitation for some patients, except for some exercises without joint load (e.g. aquagym). Other measures related to stress management (breathing exercises, meditation, yoga) have proven useful in the treatment of ETS and can also be recommended to rheumatologic patients.
Pharmacological treatment.
This is a very important chapter. The interaction of NSAIDs in the diagnosis of HT has already been mentioned. In the follow-up of hypertensive patients, these drugs, of very frequent and necessary use in rheumatic patients, can increase BP and also hinder individual control of HT, which is closely related to the prevention of vascular complications. In cases of difficult-to-control HT (the most serious case is resistant and refractory HT) this is especially serious because it requires more intense and complex antihypertensive treatment with up to 4 antihypertensive drugs of different classes to achieve the control objectives.
In this regard, attention should be paid to the interaction of NSAIDs -not steroids- with a frequent therapeutic combination in HT: ARAII or ACEI+Calcium antagonist+Diuretic, often in a single tablet with fixed doses of the three, which is widely used in clinical practice. This is known as “Triple Whammy” and can trigger very severe acute renal failure. Therefore, we must be attentive in these cases; prudence.
Article courtesy of Dr. Mariano de la Figuera, Internal Medicine Specialist. Castelldefels Medical Center