- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
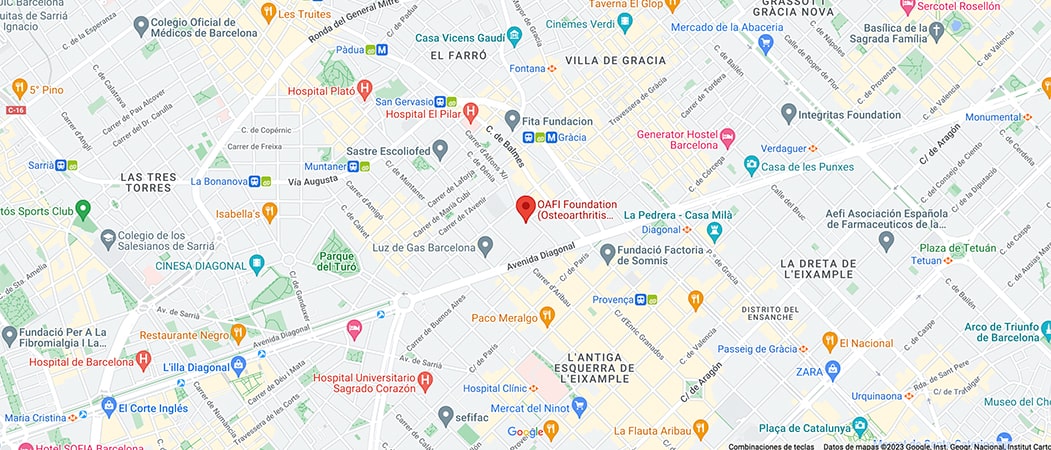
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

-

Osteoarthritis and cardiovascular diseases: a close relationship
Osteoarthritis and cardiovascular risk: What do we need to know?
- It is estimated that osteoarthritis affects 7 million people in our country. Of these 7 million, more than 2 million suffer from it together with a cardiovascular pathology.
- With the campaign #ElCorazónDeTuArtrosis, from OAFI we offer you the main tools to understand how these diseases are related and how we can treat them properly.
Osteoarthritis: Key concepts
Osteoarthritis (OA) is a chronic disease that affects the cartilage, the subchondral bone, the synovial membrane and the soft tissues of the joint. Some of the symptoms are pain, loss of mobility, muscle atrophy… which are combined with the psychological wear and tear it causes.
Furthermore, osteoarthritis does not come alone; it is often accompanied by what we call comorbidities (two or more diseases at the same time in the same patient). In a survey conducted by the OA Patients Task Force, 86% of OA patients surveyed had been diagnosed with one or more co-morbidities. Hypertension and obesity were the most common, with mental health also playing an important role.
Osteoarthritis and cardiovascular diseases
45% of annual mortality in Europe is due to cardiovascular diseases (CVD). CVD and its risk factors (obesity, hypertension, etc.) are among the most frequent comorbidities in patients with osteoarthritis. Both osteoarthritis and CVD also share risk factors (age, sedentary lifestyle, inflammation, etc.).
It is also known that patients with OA tend to have a higher number of cardiovascular risk factors such as obesity, hypertension and diabetes, among others.
On the other hand, a recent meta-analysis showed that patients with osteoarthritis have a 24% higher risk of cardiovascular disease than a patient without OA. In the case of patients with wrist osteoarthritis and CVD, studies have found that they are less likely to improve their Osteoarthritis pain.
I have Osteoarthritis and a cardiovascular disease, what should I do?
Despite the high prevalence of osteoarthritis, therapeutic options are still scarce and tend to approach the disease from a symptomatic point of view with the administration of analgesics and NSAIDs, which, depending on the patient’s profile, can cause cardiovascular, gastrointestinal, renal and hepatic side effects.
Other therapeutic alternatives are opioids (which are limited by their side effects), intra-articular drugs, which may cause discomfort in some patients, or topical NSAIDs, which are safer than oral NSAIDs for patients with cardiovascular risk.
In the case of cardiovascular comorbidity, the option of chondroitin sulphate (CS) and glucosamine (GS), two slow-acting symptomatic drugs, is particularly interesting. Despite their controversial use, the combination of CS and GS has been shown to improve pain in the short term and is associated with reduced mortality from cardiovascular causes, reducing the risk of myocardial infarction and stroke.
The Pharmacoepidemiology and Clinical Pharmacology Research Group of the University of Alcalá, led by Prof. Francisco J. de Abajo, has demonstrated through various investigations that the use of CS and GS can reduce the risk of acute myocardial infarction by 31% and the risk of ischaemic stroke by 34%.
These results suggest possible anti-inflammatory effects of CS and GS, which make them particularly effective in the treatment of osteoarthritis. Not only do they lack adverse effects, but they may also have beneficial effects at a cardiovascular level, making them an ideal choice for this disease.
It is therefore essential to know the cardiovascular risk associated with the use of the drugs used to treat osteoarthritis and to assess the cardiovascular risk of each patient, in order to administer the most appropriate treatment for their condition. Remember to always ask your doctor for the most suitable option for your case.
Osteoarthritis and CVDs: a close relationship
It is important to take into account the close relationship between osteoarthritis and cardiovascular diseases. Both diseases influence each other’s evolution and we must treat them correctly to ensure the well-being of patients.
We must not forget that we must continue to promote non-pharmacological measures that can also help us to reduce cardiovascular risk, such as a healthy diet, walking, moderate physical exercise (tai-chi, yoga, aquagym, etc.) and, above all, providing patients with the tools to better understand and manage their disease, putting them at the centre of it. It is in this area that patient associations such as OAFI play a key role.
Information extracted from the article “Osteoarthritis and cardiovascular risk: new factors to take into account”, written by Dr. Josep Vergés, president of OAFI and AECOSAR and Nina Martínez, head of R&D at OAFI.