- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
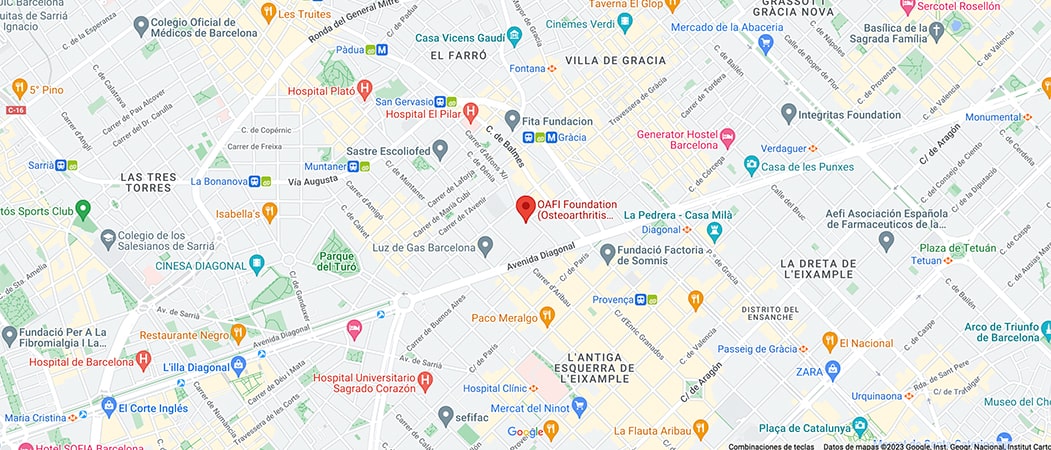
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

-

Dysphagia and Osteoarthritis: Understanding two key conditions and their relationship

Dysphagia and osteoarthritis are two medical conditions that affect different parts of the body but may have surprising interactions. This article explores their main characteristics, possible connections and treatment methods.
First of all, let’s talk about dysphagia, what is it?
The term dysphagia comes from the Greek “dys” (difficulty) and “phagia” (eating).
Dysphagia is defined as a symptom that refers to the difficulty or discomfort that occurs when forming and/or moving the food bolus from the mouth to the esophagus.
Dysphagia can be located at the oropharyngeal or esophageal level. Oropharyngeal dysphagia includes swallowing disorders of oral, pharyngeal, laryngeal and upper esophageal sphincter origin and comprises almost 80% of dysphagia diagnoses. Esophageal dysphagia refers to alterations in the upper esophagus, esophageal body and lower sphincter and accounts for 20% of diagnoses.
The populations most at risk for dysphagia are the elderly (affecting 30-40% of people aged 65 years or older), people with neurological or neurodegenerative diseases, and people with head and neck diseases. Early diagnosis and appropriate treatment are essential, as dysphagia can lead to serious complications such as malnutrition or aspiration pneumonia.
What are the symptoms of Dysphagia?
There are different signs that make us suspect dysphagia:
- Coughing or choking when eating, or immediately after, with all or any consistency, especially liquids.
- Voice changes during or after swallowing.
- Drooling, difficulty in saliva control.
- Difficulty with bolus formation and handling of food in the mouth.
- Fractionated swallowing (having the need to swallow several times to eat a small bolus).
- Swallowing food in small amounts, little by little.
- Residue in the mouth after swallowing.
- Sensation of food retention in the pharynx and the need to swallow several times.
- Coughing during or after meals.
- Excessive time spent eating.
- Progressive weight loss.
- Febrile peaks without apparent cause.
- Repeated respiratory infections (due to bronchoaspiration).
Osteoarthritis: A degenerative disease
Osteoarthritis is a chronic pathology characterized by wear and tear of the articular cartilage, which generates pain and stiffness in the joints. It is the most common form of arthritis and its prevalence increases with age. Factors such as overweight, genetics and repetitive use of certain joints increase the risk of developing it. Commonly affected joints include the knees, hips and hands.
Osteoarthritis limits quality of life and can lead to severe disability if not managed properly.

The connection between Dysphagia and Osteoarthritis
Although these two conditions appear to be unrelated, there are circumstances where they converge.
For example, cervical osteoarthritis, which affects the vertebrae of the neck, can cause compression of structures near the esophagus, causing mechanical dysphagia.
On the other hand, within cervical osteoarthritis, it can cause bony changes or the formation of osteophytes (bony growths). These structural changes can put pressure on the esophagus or the nerve pathways that control the swallowing muscles, leading to mechanical dysphagia.
In these cases, swallowing difficulty is not caused by neurological problems, but by a physical obstruction or structural alteration.
In addition, older adults, commonly affected by osteoarthritis, are also more prone to dysphagia due to the natural aging of the muscles involved in swallowing.
What should I do if I suspect I have dysphagia?
If dysphagia is suspected, we should see an otorhinolaryngologist specialized in dysphagia to make the diagnosis.
We should also see a speech therapist specializing in dysphagia for guidance on what type of food we can eat and to help us with the rehabilitation of dysphagia.
In conclusion, we can say that both dysphagia and osteoarthritis present significant challenges, but research continues to provide better approaches to their management. Understanding the relationship between these two conditions is crucial to developing comprehensive and personalized treatments.
Bibliographic References
- Velasco MM, Arreola V, Clavé P, Puiggrós C. Abordaje clínico de la disfagia orofaríngea: diagnóstico y tratamiento. Nutr Clin Med. 2007; 1 (3): 174-202.
- WGO. Disfagia. Guías y cascadas mundiales. Vol. 1. World Gastroenterology Organisation; 2014. p. 55-72.
- Hochberg, M. C., Altman, R. D., April, K. T., et al. (2012). American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research, 64(4), 465–474.
- Hunter, D. J., & Felson, D. T. (2006). Osteoarthritis. BMJ, 332(7542), 639–642.
- Katz, P., Yelin, E., & Haaz, S. (2014). Prevalence and correlates of perceived employment discrimination among working-age adults with arthritis. Arthritis Care & Research, 66(9), 1306–1313.
- Logemann, J. A. (1998). Evaluation and Treatment of Swallowing Disorders. Austin: Pro-Ed.
- Smithard, D. G., O’Neill, P. A., England, R. E., et al. (1996). The natural history of dysphagia following a stroke. Dysphagia, 11(4), 231–237.
- Atenció a la disfàgia orofaríngia en els diversos àmbits del sistema de salut Document de consens Octubre de 2018
Recover now our OAFI Radio show (in Spanish), about DYSPHAGIA, SARCOPENIA AND NUTRITION: HOW CAN FOOD HELP US?
In the show of #OAFIRADIO we explore dysphagia and what nutritional alternatives exist to anticipate or manage this pathology, such as modified textures, with Natàlia Talleda, speech therapist and occupational therapist, and Patricia Sanz, Campofrío Food Group, as well as Susana’s testimony. In addition, together with the nutritionist Antonela Bávaro, we know how nutrition can help us to strengthen our muscles and prevent or improve pathologies such as sarcopenia.